What is Keratoconus?
Keratoconus is a progressive condition where the front window of the eye (the cornea) is shaped like an irregular rugby ball as opposed to a football. This is a more extreme and irregular form of astigmatism than that which is typically found throughout the population. This extreme degree of astigmatism distorts the vision and can be difficult to correct with spectacles. Keratoconus is derived from the Greek words: kerato, meaning cornea, and konos, meaning cone. The cornea becomes distorted by a cone-shaped bulge which occurs as a result of thinning and forward protrusion of the central/paracentral region.
Keratoconus affects about 1 in 2000 of the population, presenting typically in teenage years or in the early 20s. It is the commonest reason for corneal transplantation in this age group. Progression of the condition depends on many factors including the age at the time of the onset. The younger the age, the faster keratoconus progresses.
The condition almost always affects both eyes, with one eye usually more affected than the other.
The precise cause of Keratoconus is unknown. We do know that there are several risk factors for its development including: hereditary factors, excessive eye rubbing, certain underlying disorders such as Downs Syndrome. Affected patients often suffer from allergic eye disease.
Your eye surgeon will need additional information both when assessing you for the first time, and also for ongoing monitoring. This includes refraction data (your spectacle or contact lens prescription) and corneal topography scans.
Corneal topography is a very sensitive way of documenting even early keratoconus.
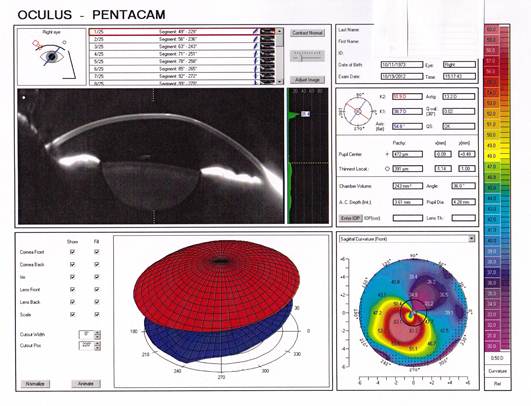
In more obvious cases, such as that shown here, the scan illustrates inferior paracentral bowing forward & steepening of the cornea and associated thinning.
Keratoconus can be managed with a variety of techniques including the following:
- Spectacles in the early stages of the disorder
- Hard contact lenses when spectacles are no longer helpful
- Corneal collagen cross linking (CXL) with Riboflavin which increases the strength of the cornea to prevent progression of the keratoconus
- Intrastromal rings (Intacs)
- Keraflex (Microwave Thermoplasty)
- Corneal transplantation - deep anterior lamellar keratoplasty (DALK) or full thickness penetrating keratoplasty (PK) for more advanced stages.
Until relatively recently, there was no way of arresting the progression of Keratoconus and similar conditions.
This is a technique which uses an intense ultraviolet light (UVA) source and a photosensitising chemical (Riboflavin) to create increased linkages (cross-linking) between the cornea’s collagen fibres. This technique has been shown to be extremely successful in arresting the progression of (stabilising) the condition and occasionally even producing small improvements.
Procedure Overview
Your surgeon will place anaesthetic drops in the eye to be treated and then an eyelid holder in your eye to keep it open throughout the procedure. A thin surface sheet of cells is marked by a manual cutting ring, a small amount of alcohol is then applied over this sheet to loosen it and thus enable the surgeon to roll it away from the area to be treated. The eye is then soaked in riboflavin eye drops (2 drops every 2 minutes for 10 - 20 minutes). An ultraviolet (UVA) light is then shone on the cornea for 2 - 5 minutes and the procedure is complete. You will have some drops placed in your eye and a contact lens may be fitted. This lens is for protection as well as aiding in reducing discomfort. The whole procedure usually takes about 20 - 40 minutes.

Aftercare
After the procedure is completed, you will be given a full explanation regarding post-operative drops and tablets and follow up care. Protective eye shields will have been placed over the treated eye to prevent you from rubbing your eye for the rest of the day and also whilst sleeping during at night.
During the early post-operative period it is important not to squeeze or rub the eyes. Antibiotic and anti-inflammatory drops are used to prevent infection and decrease inflammation.
After leaving the clinic, patients are encouraged to rest/sleep for a few hours. The majority of patients will have moderate to severe discomfort beginning a few hours after the crosslinking procedure and this usually disappears within 24 - 48 hours. However, to ensure that the majority of patients have as comfortable a period after treatment as possible, all patients are given painkilling tablets to be taken every 4 – 6 hours for 24 – 48 hours.
A post operative follow up appointment takes place at the clinic approx. 7 days after the procedure, to ensure that your eye is healing as expected. There are a few restrictions for a week or so following your procedure, but as long as you follow your doctor’s instructions, you should be free to resume all of your normal activities thereafter.
Although KXL is a short procedure, you have had an operation and should therefore try to rest and relax for the first 24 – 36 hours after treatment. The best plan is to slightly darken a room and listen to some music, rather than trying to read or watch television. (Both reading and watching television can cause your eye to move under the patch and may make the discomfort greater.)
Who does the condition affect?
Typically young adults or teenagers. There is an association with atopic, or allergic-type, conditions and when there is a family history of the condition.
What causes Keratoconus?
The precise cause of Keratoconus is unknown. We do however, know that there are several risk factors for its development. These include: hereditary factors, excessive eye rubbing, certain underlying disorders such as Downs Syndrome. Affected patients often suffer from allergic eye disease.
Can Keratoconus be prevented?
There is no known prevention for this condition. However, there are good treatments to manage the condition and now we have advanced techniques (Collagen Cross-linking) to slow down the progression of the disease process.
Who is suitable for treatment?
Anyone who has progressive keratoconus may be suitable. Those patients with advanced keratoconus or severe scarring may not be suitable for treatment, especially if they have poor vision with contact lenses.
Is cross-linking a cure for Keratoconus?
Crosslinking is extremely successful in arresting the progression of Keratoconus. Studies have shown a success rate of more than 95% of those who have been treated. Whilst it is not a cure for the condition, it is likely to prevent the need for more invasive surgery such as corneal transplant.
What is the difference between your technique and traditional cross-linking? - Our accelerated crosslinking procedure takes on average 30 minutes to complete. This compares to approx. 90 minutes for the ‘traditional’ method, which is no more effective.